Progress in Bronchiectasis Research: Acute Exacerbation of Bronchiectasis Closely Related with Acute URTI
2023-05-221467Bronchiectasis is a common chronic airway suppurative disease in adults. Recurrent airway infections, inflammation and incomplete reversible airway dilation are its main pathogenesis. Acute exacerbation is an important clinical event in the progression of bronchiectasis, and frequent acute exacerbation often leads to poor prognosis. Prevention of acute exacerbation is an important part of bronchiectasis administration. Pathogens are often isolated from bronchiectasis patients. Previous studies have revealed that bacteria are closely related to the occurrence and progression of bronchiectasis. As a common pathogen in the respiratory tract, the virus is a trigger for acute exacerbation of bronchiectasis and may drive its progression. However, the role of viral infection in acute exacerbation is still unknown.
Acute upper respiratory tract infection (URTI) is usually a self-limiting disease, which is mainly triggered by the infection of opportunistic pathogens (especially respiratory viruses). Viruses are often detected in different chronic airway diseases and can trigger the acute exacerbation of chronic airway diseases. About half of the asthma attacks were associated with URTI caused by rhinovirus infection. In acute exacerbation of chronic obstructive pulmonary disease (AECOPD), URTI symptoms were reported in 83% of patients and virus was detected in 44% of URTI patients. In AECOPD, patients with virus detected URTI showed the most significant increase in respiratory symptom burden when compared with those reported with URTI alone or detected with virus alone. Frequent exacerbators of COPD have a more frequent history of URTI, and URTI events also increase the risk of AECOPD occurrence.
A series of research findings of the research team have demonstrated that respiratory viruses are common detected pathogens in bronchiectasis patients (Chest.2015; Arch Bronconeumol.2020; Open Forum Infect Dis.2020) and bacterial shifting (such as detection of new pathogenic bacteria) is often associated with acute exacerbation. Patients with acute exacerbation detected with both viruses and bacteria suffer a heavier burden of upper respiratory tract symptoms. However, the relationship between URTI and bronchiectasis has not been clarified. This study aims to study the patients with URTI in acute exacerbation: (1) the pathogen spectrum of lower airway, (2) symptom burden, (3) duration of recovery, and (4) the risk of acute exacerbation in the future. The study also aims to identify the cardinal pathogens in the acute exacerbation of bronchiectasis, clarify their association with URTI, and advocate timely identification and prevention of URTI to reduce the risk of acute exacerbation of bronchiectasis in the future.
In this study, acute exacerbation events are classified by whether URTI also occurs with acute exacerbation into URTI-AE and non-URTI-AE. By the onset time of URTI, URTI-AE is classified into two subgroups: early onset URTI-AE (acute exacerbation within 3 days after the occurrence of URTI) and late onset URTI-AE (acute exacerbation within 4-21 days after the occurrence of URTI) (Figure 1). Sputum samples from patients with acute exacerbation during onset and recovery were collected to perform common viral PCR testing, bacterial culture and inflammatory factors detection; blood samples were collected for the detection of systemic inflammation markers. Three symptom questionnaires (BEST, CAT, EXACT), which have recently been developed or verified by foreign researchers to be able to accurately and sensitively identify the acute exacerbation of chronic airway disease patients (including bronchiectasis), were used to evaluate the symptom burden of patients in acute exacerbation stage. Patients were followed up to collect their history of acute exacerbation within the next year. Finally, the differences in pathogen spectrum, symptom burden, recovery duration, and future risk of acute exacerbation were compared between URTI-AE and non-URTI-AE groups and between different subgroups.
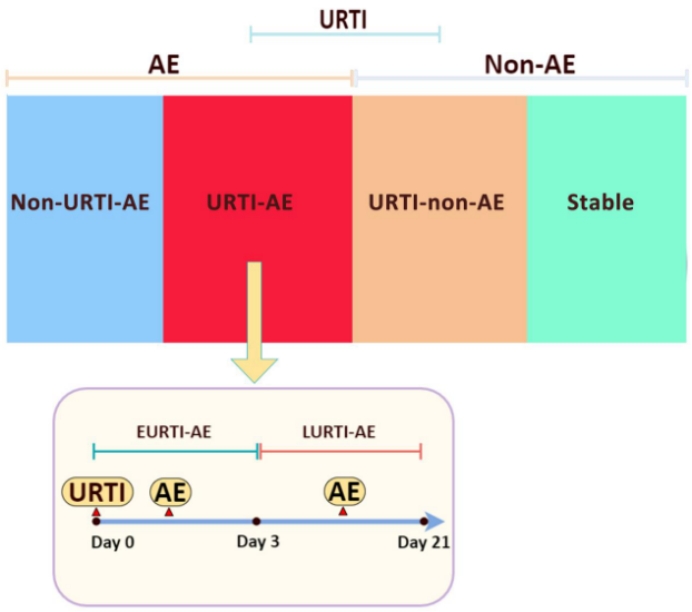
Figure 1. Research grouping
URTI-AE: URTI-related acute exacerbation group; Non-URTI-AE: non-URTI-related acute exacerbation group; EURTI-AE: acute exacerbation within 3 days after the occurrence of URTI; LURTI-AE: acute exacerbation within 4-21 days after the occurrence of URTI; Stable: Stable stage.
A total of 89 URTI-AE cases and 81 non-URTI-AE cases were included in this study. The virus detection rate was significantly higher in the URTI-AE group than that in the non-URTI-AE group (46.1% vs.4.9%, P <0.001, Figure 2). A higher proportion of patients were detected with new bacterial strains in the URTI-AE group. In the airway pathogen spectrum, rhinovirus, influenza virus and coronavirus were mainly detected in both groups, while metapneumovirus and herpes simplex virus were unique to the URTI-AE group. Total load of viruses in the URTI-AE group [Ct: 40.0 (29.6-40.0) vs. 40.0 (33.9-40.0), P <0.001], and loads of multiple viruses were significantly higher in URTI-AE group than those in the non-URTI-AE group. The viral spectrum and viral load were similar between EURTI-AE and LURTI-AE groups (Figure 3). Rhinovirus detection was significantly associated with the occurrence of URTI-AE (odds ratio: 5.00, 95% confidence interval: 1.06-23.56, P =0.03). There was no significant difference in airway (IL-1 β, IFI 27, etc.) and systemic (blood routine, CRP, etc.) inflammation indicators between the two groups.
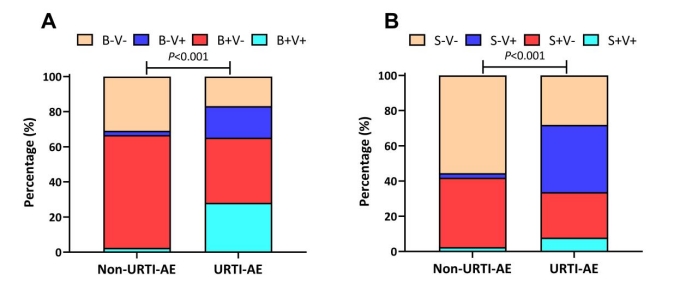
Figure 2. Overall detection results of URTI related / non-URTI related acute exacerbation pathogens
B+V+: both bacteria and virus detected; B+V-: bacteria detected but no virus detected; B-V+: virus detected but no bacteria detected; B-V-: neither bacteria nor virus detected. S+V+: bacterial spectrum shifting with virus detected, S+V-: bacterial shifting but no virus detected; S-V+: no bacterial shifting with virus detected; S-V-: neither bacterial shifting nor virus detected.
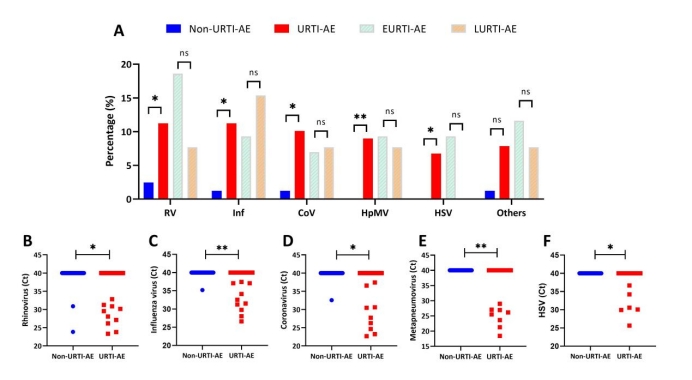
Figure 3. Virus spectrum of acute exacerbation associated with URTI
RV: rhinovirus; Inf.: influenza virus; CoV: coronavirus; HpMV: human metapneumovirus; HSV: herpes simplex virus; Others: parainfluenza virus, bocavirus, respiratory syncytial virus, enterovirus, adenovirus.
As assessed by the three symptom questionnaires, the symptom burden of the URTI-AE group was significantly heavier than that of the non-URTI-AE group during the onset and recovery stages. The URTI-AE group required a longer recovery period (7 days vs. 4 days, Figure 4).
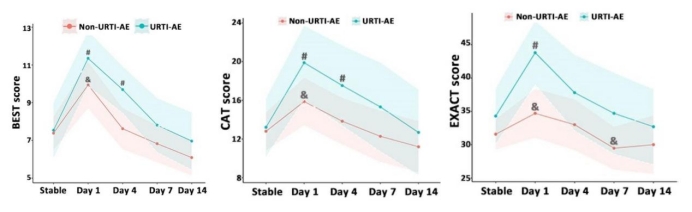
Figure 4: Symptom load of URTI-related acute exacerbation
BEST, CAT, EXACT: The scores of the three symptom questionnaires; Stable: stable stage; Day1: first visit for acute exacerbation (onset); Day 4, 7, 14: recovery visit for acute exacerbation (Day 4, 7, 14). #: P<0.05 denoted statistically significant difference in the score between AE onset or the time points after the onset of AE compared with stable status in URTI-AE. &: P<0.05 denoted statistically significant difference in the score between AE onset or the time points after the onset of AE compared with stable status in non-URTI-AE.
Compared with non-URTI-AE group, there is no significant difference in the frequency of acute exacerbation occurring to URTI-AE group in the future, but with a higher risk in the recurrence of URTI-AE (odds ratio: 10.90, 95% confidence interval: 3.60-33.05, P <0.01; transition probability in Markov chain model: 0.78, Figure 5).
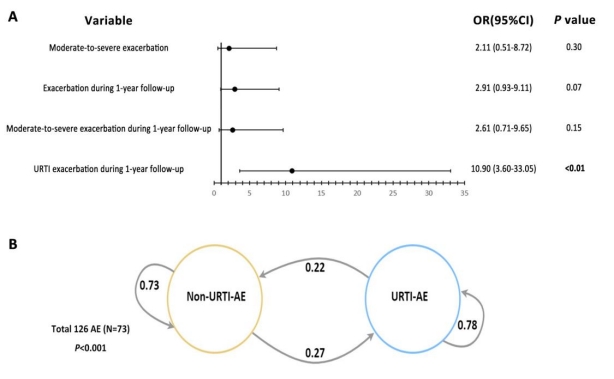
Figure 5. URTI and association with acute exacerbation of bronchiectasis and transition probability
(A) Comparison of the proportions of various types of acute exacerbation between URTI-AE and non-URTI-AE groups (GEE model);
(B) The transition probability of a different type of acute exacerbation between URTI-AE and non-URTI-AE groups (Markov-chain model).
According to the results of this study, in acute exacerbation in bronchiectasis patients, compared with the non-URTI-AE group, the URTI-AE group is characterized by a broader pathogen spectrum, higher viral load, heavier clinical symptoms, longer recovery time, and increased risk of poor prognosis. Prevention and treatment of URTI may have important benefits for bronchiectasis patients.