National multi-center study establishes a prediction model for adverse maternal and foetal/neonatal outcomes in pulmonary hypertension
2022-11-251115
Pulmonary hypertension (PH) is a fatal and progressive disease. It is estimated that the global prevalence of pulmonary hypertension is about 1%, and the prevalence of pulmonary hypertension among the population aged over 65 is as high as 10%. There are about 12 million PH patients in China. Some of them are fertile women or patients newly diagnosed with pulmonary hypertension after developing symptoms during pregnancy. Women with a history of pulmonary arterial hypertension (PAH) and other forms of severe PH, after getting pregnant, have a maternal mortality rate of 56% and a neonatal mortality rate of 13%. Therefore, multiple clinical guidelines recommend strict contraception and termination of pregnancy for women with pulmonary hypertension. Maternal mortality rate has decreased with improvements in PAH treatment and progress in management methods for women in gestational and perinatal stages. In addition, many female patients have a strong desire to have a baby, so the 2022 ESC diagnosis and treatment guideline for pulmonary hypertension gives more specific suggestions for this group of patients, emphasizing individual patient assessment and doctor-patient decision-making. Therefore, establishing a scientific predictive model for them is conducive to individualized risk assessment of patients, and will provide a reliable auxiliary tool for clinical decision-making.
National Center for Respiratory Medicine, the First Affiliated Hospital of Guangzhou Medical University, Guangzhou Institute of Respiratory Health and the SKLRD’s pulmonary vascular orientation director, professor Wang Jian led his team to organize a national multi-center clinical research, which collected clinical information of pregnant patients with PH and made follow-up visits, established a predictive model for the adverse maternal and foetal/neonatal outcomes to provide a scientific tool for assisting clinical decision-making and prenatal counseling. The related paper entitled “Prediction and prognosis of adverse maternal and foetal / neonatal outcomes in pulmonary hypertension: an observational study and nomogram construction” was published online in the journal Respiratory Research on November 15, 2022 (JCR: Q1, IF: 7.16).
A total of 693 patients were included by the study in 6 sub-centers across the country, which collected their clinical information and made follow-up visits to determine their clinical outcome and survival. The adverse clinical outcomes of pregnant women were defined as death or heart failure. adverse clinical fetal / neonatal outcomes were defined as: fetal death, neonatal death within 30 days after birth, and small for gestational age infant (SGA). Of these patients, 420 belonged to training cohort and 273 belong to validation cohort. The results revealed that type I respiratory failure, NYHA cardiac function grade, N-terminal brain natriuretic peptide precursor ≥ 1400 ng/L, arrhythmia, and eclampsia with previous hypertension were independent risk factors for maternal death or cardiac failure. Type I respiratory failure, arrhythmias, caesarean section under general anesthesia, NYHA cardiac function grade, and the N-terminal brain natriuretic peptide precursor ≥1400 ng/L were independent predictors of survival rate of women with pulmonary hypertension during pregnancy. For fetal / neonatal adverse clinical events, type I respiratory failure, arrhythmia, caesarean section under general anesthesia, parity, platelet count, fibrinogen, and left ventricular systolic diameter were important predictors. The nomogram developed on this basis for the prediction of maternal adverse clinical outcomes, adverse fetal / neonatal outcomes and long-term prognosis of patients showed a good performance of identification and calibration in training and validation cohorts, and online prediction tools were developed and released for clinical application and promotion.
The corresponding authors of the study are Professor Wang Jian and Professor Liu Chunli with the SKLRD ,Professor Cheng Zhe from the First Affiliated Hospital of Zhengzhou University, Professor Zhang Jun, director of Beijing Anzhen Hospital, Capital Medical University, and Professor Luo Yiping, director of Guangdong Maternal and Childcare Hospital. The first authors are Chen Yuqin, associate researcher of the SKLRD, Master Zhou Dansha, Xiong Mingliang, director of the Third Affiliated Hospital of Guangzhou Medical University, Xi Xin, director of Beijing Anzhen Hospital, Capital Medical University, Zhang Wen’ni, director of Guangdong Maternal and Childcare Hospital, and Zhang Ruifeng, director of the Zhongda Hospital Southeast University. The project is supported by the programs such as National Natural Science Foundation of China, the National Key Research and Development Program, and the independent project of the State Key Laboratory of Respiratory Diseases.
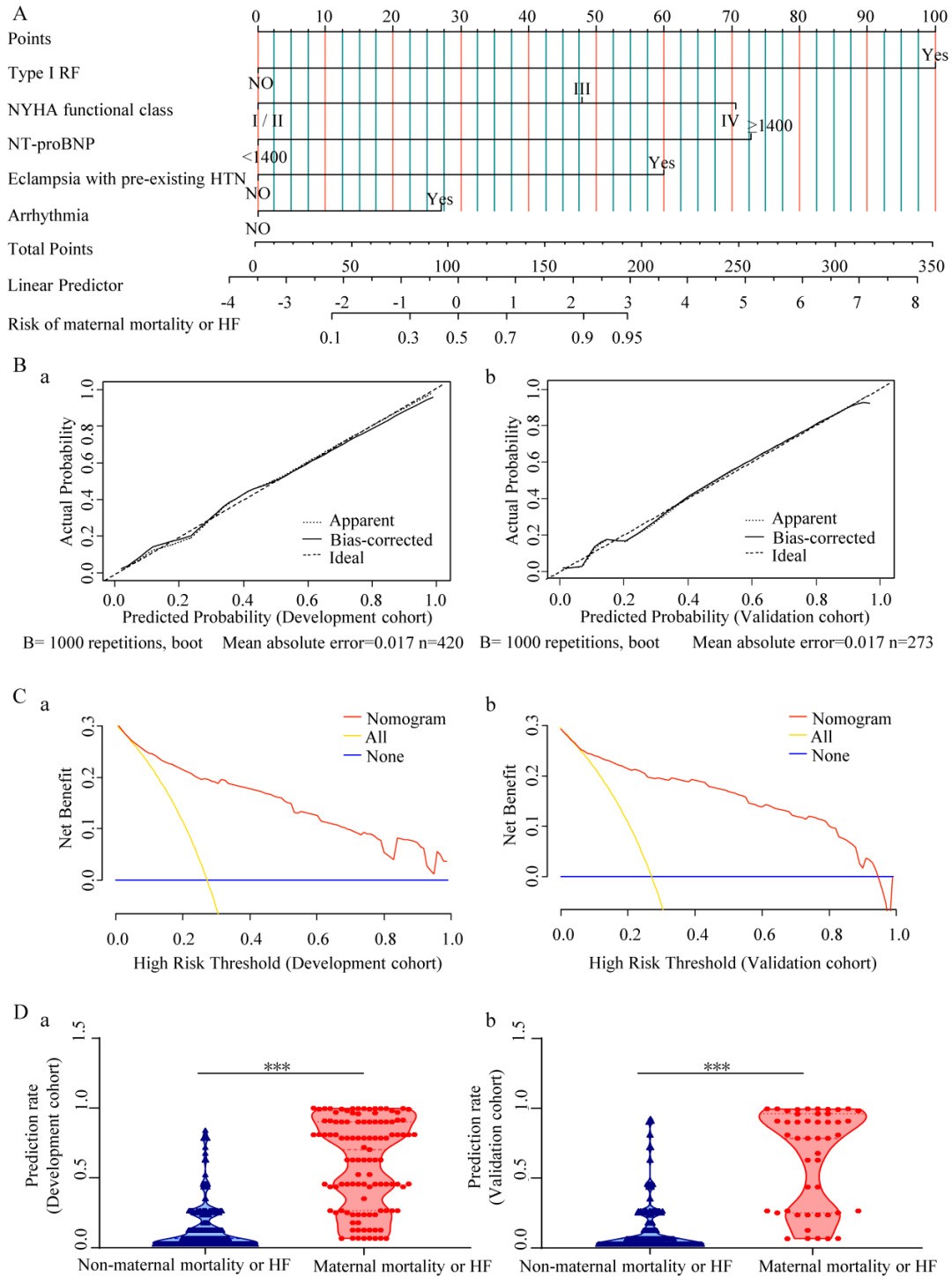
Fig. 1: The nomogram established in this study for the prediction of the adverse clinical outcomes of pregnant women with PH
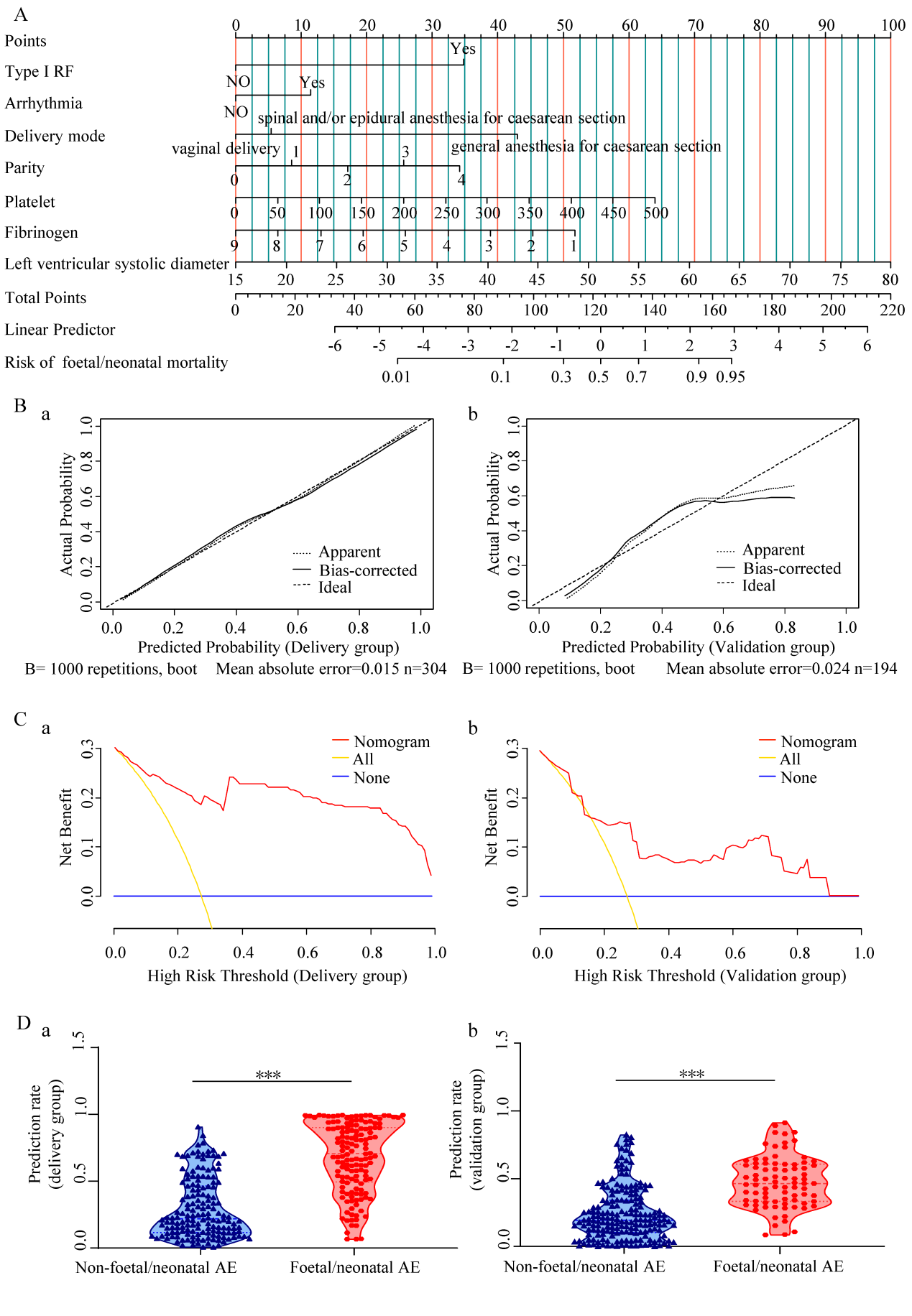
Fig. 2: The nomogram established in this study for the prediction of foetal/neonatal adverse clinical outcomes
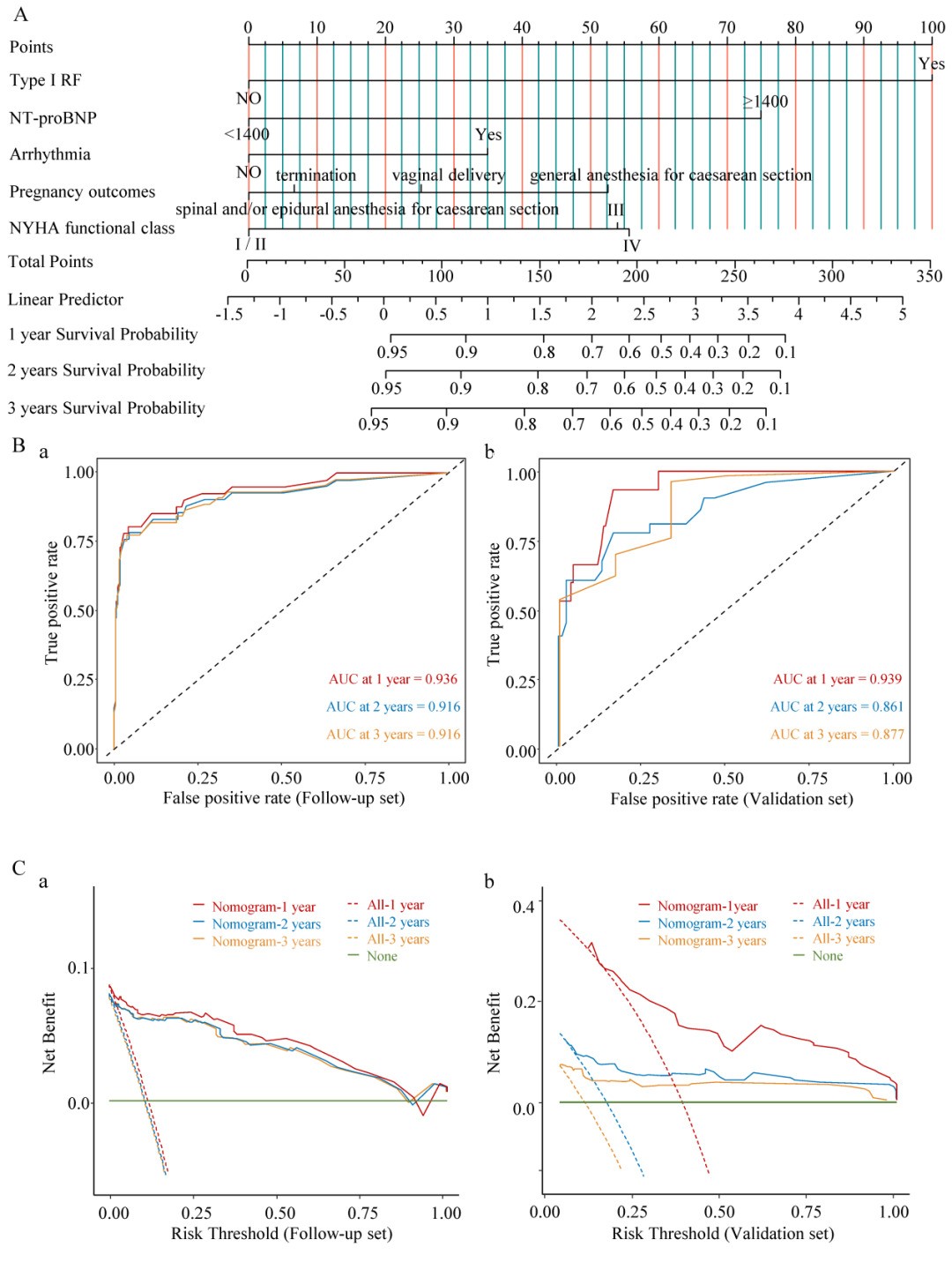
Fig. 3: The nomogram established in this study for the prediction of long-term survival of pregnant women with PH
Original paper:https://respiratory-research.biomedcentral.com/articles/10.1186/s12931-022-02235-y